
Dental implants can be a life-changing solution if you have missing teeth, but only if you care for them properly. Neglecting your new pearly whites can lead to serious issues down the road. Even if your Mira Mesa dentist and implant specialist is reliable and experienced, the maintenance is up to you once you leave their office.
With a few simple professional tips and information, you should have no trouble at all. Let’s go over the nine most common mistakes that people make with their dental implants. Keep your new smile bright, healthy and trouble-free. Your future self will thank you.
Are dental implants hard to maintain?
Your new smile requires a similar level of care as natural teeth. Unlike natural teeth, they don’t decay, but the surrounding gum tissue and bone are still vulnerable to infection. This means that you should never skip the cleaning. While this should be simple, some people can find dental implants maintenance more challenging due to certain factors. For example, if you have difficulty reaching certain areas of your mouth, you might need specialized tools or techniques.
This routine isn’t complex, but it does require some diligence, awareness and a commitment to your overall health. If you’re proactive and follow your dentist’s recommendations, your new smile can last a lifetime.
What are common mistakes in dental implant maintenance?
Let’s go over the 9 most common mistakes when it comes to maintaining your new smile:
1. Skipping regular check-ups
Your new teeth, like natural teeth, need professional attention. Regular check-ups allow your dentist to monitor the health of your new implant-supported teeth and surrounding tissues. They will check for signs of inflammation, infection, or bone loss, which can compromise stability.
Professional cleaning removes plaque and tartar buildup, reducing the risk of per-implantitis (an infection around the implant). Aim to schedule your check-ups and cleanings every six months, or as recommended by your dentist.
2. Neglecting daily hygiene
Plaque and bacteria can accumulate on and around your new teeth, just like natural teeth. Inadequate oral hygiene can lead to inflammation, infection, and even failure. Maintenance of dental implants includes brushing your teeth twice a day with a soft-bristled brush and non-abrasive toothpaste. Floss daily using interdental brushes or floss threaders to reach tight spaces. This daily routine will prevent plaque from building up.
3. Ignoring signs of trouble
Be vigilant about any changes around your new teeth. Bleeding or swollen gums, pain, difficulty chewing, or a loose tooth should not be ignored. These could indicate peri-implantitis, a bacterial infection that can damage the bone supporting the new tooth. If you notice any of these symptoms, don’t delay, reach out to your clinic immediately. Early intervention can often prevent future damage.
4. Using your teeth as tools
Your new teeth are not meant to be used as tools. Avoid using them to open packages, bottles, or for any other purpose besides eating and speaking. Biting on hard objects like ice, hard candy or nuts can also damage or loosen your new teeth. Treat them with the same care you would give to your natural teeth.
5. Smoking and excessive alcohol consumption
When it comes to dental implants, care and maintenance can be more complicated if you’re a smoker. Smoking is a major risk factor for failure. It impairs blood flow to the gums and jawbone, which can hinder healing and osseointegration (the fusion with the bone).
Smokers are also more prone to infection and gum disease, both of which can compromise the success of the procedure. Similarly, too much drinking can dehydrate your mouth, which increases your risk for oral health problems. If you smoke or drink heavily, consider reducing or quitting for the sake of your new smile.
6. Not wearing a nightguard
If you grind your teeth at night, a custom-fitted nightguard is crucial to protect both your natural teeth and your new additions. The excessive force from grinding can damage your new teeth, loosen them, or even cause fractures. Talk to your dentist about getting a nightguard to prevent these problems and make your new smile last as long as possible.
7. Neglecting your overall health
Your oral health can depend on your general health and vice versa. Certain medical conditions, like uncontrolled diabetes, can increase the risk of failure. If you maintain a relatively healthy lifestyle, including a balanced diet and regular exercise and you manage any underlying medical conditions, your procedure is likely to work. Remember, a healthy body supports healthy gums and bones, which are the key to your new smile.
8. Not following post-operative instructions
After your procedure, you need to carefully follow your surgeon’s specific guidelines for healing. This may include avoiding certain foods, using prescribed mouth rinses, and taking any necessary medication. Ignoring these instructions can lead to a variety of health issues, including complications, infections and even procedure failure.
9. Having an unhealthy diet
Your diet plays an important role in keeping your bones and gums healthy. Both your bones and gums are very important for the success of your procedure. A diet high in sugar and processed foods can fuel inflammation and gum disease. This can potentially jeopardize your new teeth. Instead, focus on nutrient-rich foods like fruits, vegetables, lean protein, and dairy, which promote oral health and overall well-being.
Where in Mira Mesa and the surrounding area can I find high-quality All-on-4 dental implants?
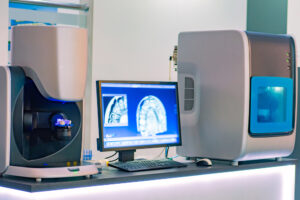
Tired of dealing with the limitations of traditional dentures? At Temecula Center for Dental Implants, we offer a permanent, natural-looking solution for your teeth. Our dedicated and qualified Dr. Tsvetov uses the latest advancements in the field to deliver exceptional results. Our comprehensive approach incorporates 3D imaging, computer-guided surgery, and biocompatible materials to ensure your new teeth are placed with precision and seamlessly integrate with your jawbone.
This means a faster recovery, reduced discomfort, and a beautiful, long-lasting smile that looks and feels like your own. Whether you live close to Los Peñasquitos Canyon Preserve or in another part of Mira Mesa, don’t worry, we’re just a quick ride away. Reach out today to book your first consultation and see what our reliable doctor can do for you.





 Is All-on-4 better than snap-on dentures?
Is All-on-4 better than snap-on dentures? How do I find a reliable dental implants specialist in Scripps Ranch and the surrounding area?
How do I find a reliable dental implants specialist in Scripps Ranch and the surrounding area?
 How long can you leave snap-in dentures in?
How long can you leave snap-in dentures in? How can I find an experienced dental implants specialist in Scripps Ranch, CA and the surrounding area?
How can I find an experienced dental implants specialist in Scripps Ranch, CA and the surrounding area?
 Who is the leading dental implants specialist in Scripps Ranch?
Who is the leading dental implants specialist in Scripps Ranch?
 Where can I find a trusted dental implants specialist in Scripps Ranch?
Where can I find a trusted dental implants specialist in Scripps Ranch? The first step in tackling an issue is to spot the signs of an implant emergency quickly. So, here are some of the common indicators:
The first step in tackling an issue is to spot the signs of an implant emergency quickly. So, here are some of the common indicators: Where can I find a reliable dental implant specialist in Poway & the region?
Where can I find a reliable dental implant specialist in Poway & the region? The first modern dental implants were crafted from titanium, prized for its strength and lightweight nature, non-toxicity, alongside its remarkable ability to
The first modern dental implants were crafted from titanium, prized for its strength and lightweight nature, non-toxicity, alongside its remarkable ability to  Who offers the finest dental implants in Poway & the area?
Who offers the finest dental implants in Poway & the area?
 Temecula Center for Dental Implants is here to help you leave any worries about missing teeth behind. Our seasoned oral surgeon and specialist, Dr. Tsvetov, is dedicated to providing solutions that improve both your oral health and quality of life.
Temecula Center for Dental Implants is here to help you leave any worries about missing teeth behind. Our seasoned oral surgeon and specialist, Dr. Tsvetov, is dedicated to providing solutions that improve both your oral health and quality of life. 
 Do you want to restore your smile and protect your facial structure? Temecula Center for Dental Implants is here to help you get a healthy, fully functional, and aesthetically pleasing smile. Our experienced oral surgeon and implant specialist Dr. Tsvetov, is dedicated to providing state-of-the-art
Do you want to restore your smile and protect your facial structure? Temecula Center for Dental Implants is here to help you get a healthy, fully functional, and aesthetically pleasing smile. Our experienced oral surgeon and implant specialist Dr. Tsvetov, is dedicated to providing state-of-the-art