All-on-4 and snap-in dentures both aim to solve the same problem: replacing several missing teeth with a comfortable and natural-looking solution. But this is where the similarities end, and snap-ins always lose when compared to high-quality dental implants in Vista, CA.
If you’ve worn traditional dentures, you probably know all about their downsides, from sore spots and discomfort to a constant dread of whether they will move when eating or talking. If we take all this into account, it becomes clear that All-on-4 implants represent a serious upgrade that can transform your quality of life.
Looking for an all-on-4 vs snap-in dentures comparison? Well, we think that this is not a relevant dilemma, and the experiences of our patients and peers seem to back us up. In today’s article, we aim to settle this once and for all and show all the advantages of dental implants compared to snap-in dentures.
What is the difference between All-on-4 & traditional dentures?
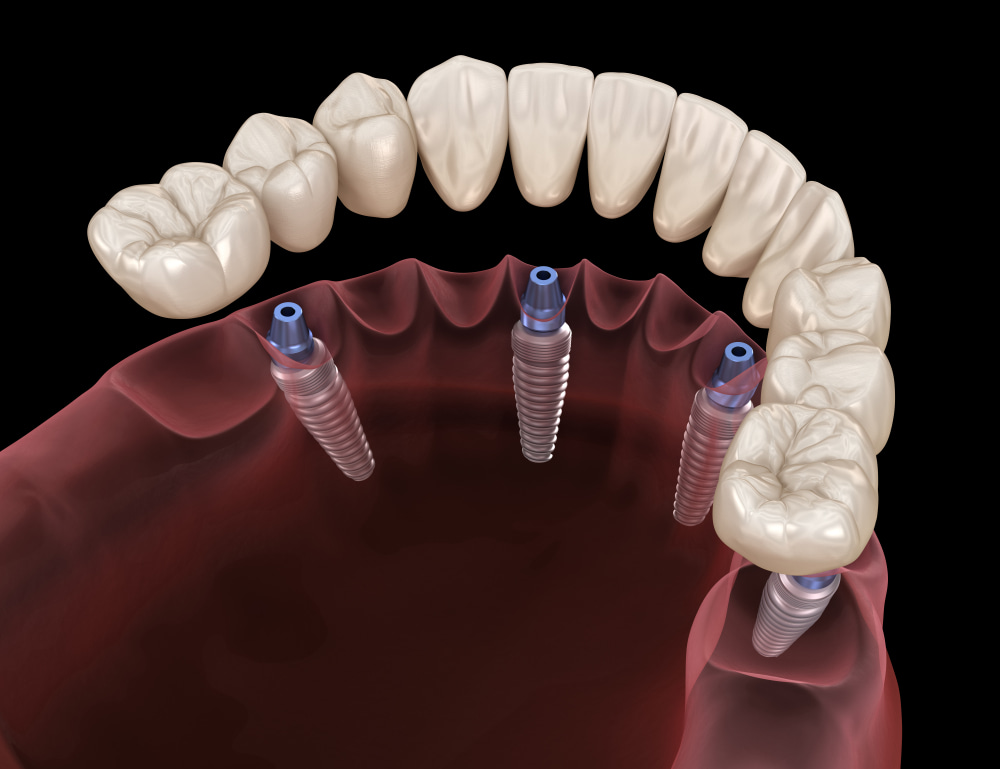
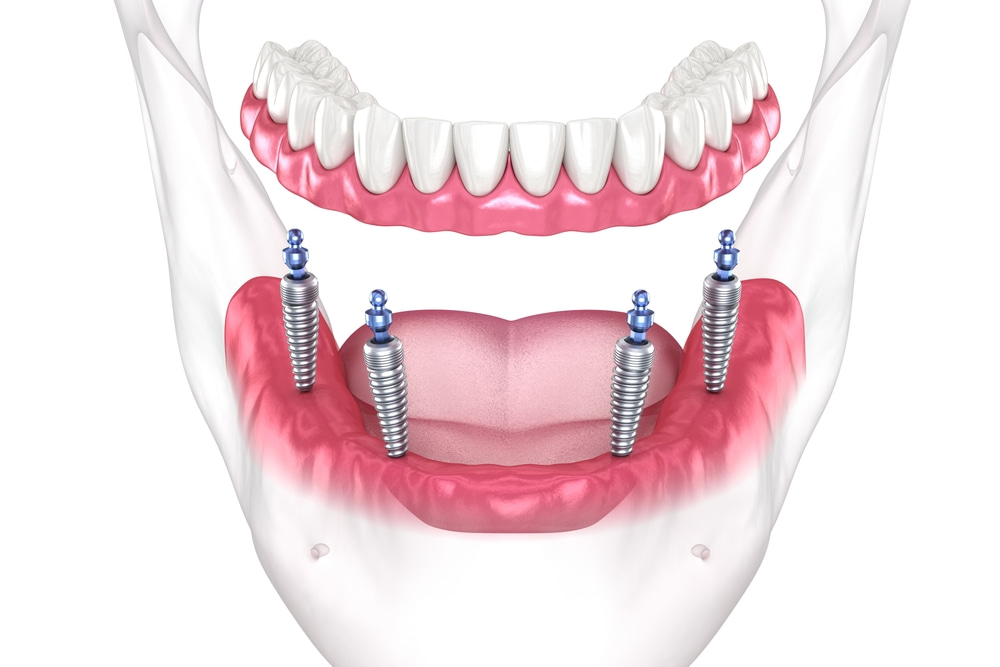
Traditional dentures rest on gums and rely on suction power, adhesives, and the shape of the ridge to stay in place. All-on-4, on the other hand, offers a full arch restoration by inserting 4 angled implants directly into the jawbone. While snap-ins can lead to slipping and discomfort, and the jawbone keeps changing over time, dental implants offer a stable foundation that doesn’t exert so much pressure on your gum tissue.
Are All-on-Four implants better than dentures?
Besides being anchored more firmly and built to last a lifetime, All-on-4 offers numerous other advantages that can significantly elevate your daily experience and simplify your routine. Whether you’re interested in a more natural look and feel, stronger bite force when eating firm foods, or you’re tired of taking out and cleaning your dentures, the reasons to choose All-on-4 are many.
Here’s how and why dental implants stand apart:
1. A truly fixed solution
As we’ve mentioned already, maybe the most noticeable difference is that All-on-4 implants are fixed and not meant to be removed. That means you don’t have to take them out at night, snap them off for cleaning, or worry about the base shifting under excess pressure. This makes biting and chewing feel more natural, strong, and comfortable.
2. Better stability = more chewing force

3. A lot less maintenance & wear
Snap-ins use attachments that wear down over time. While these parts can be tightened, relined, or replaced, they just add to more visits to the dentist that we all want to avoid. All-on-4 dental implants are not maintenance-free, but neither are your natural teeth. In fact, upkeep on dental implants is in many ways similar to what you would do for your teeth. This means regular cleaning, good hygiene habits, and occasional checkups at the dentist.
4. Improves jawbone health
One of the biggest drawbacks of traditional dentures is that they don’t stimulate the jawbone, and it will slowly start to deteriorate. Since dentures rest on gums, your bone starts feeling useless and continues shrinking over time. This can change your facial shape, reduce bridge height, and affect your appearance and oral health. On the other hand, All-on-4 implants are placed to maximize bite force and transfer load distribution through the implants onto your jawbone while you’re eating. This will preserve your facial structure and oral wellbeing.
5. Fewer pressure points & less irritation
Speaking of force, constant pressuring of your gum tissue can create friction. If the base is not perfectly aligned with the anatomy of your mouth, sore spots can start appearing as early as the adaptation period. Relining will help, but it’s a cycle you wish to avoid. With All-on-4, the prosthesis is implant-supported, so patients feel less rubbing and more comfort with every bite. They also feel and look more natural while you’re talking. This is a significant benefit that greatly improves your daily life and leads to less discomfort and everyday concerns.
6. Mimics the look of your natural teeth
One of the advantages that snap-in dentures can’t match is the aesthetic appearance. Some patients don’t like handling their dentures, feel awkward displaying them during social interactions, and even lose confidence or self-esteem when their peers become aware that they have snap-ins. Since All-on-4 dental implants are anchored and you don’t have to remove them, they don’t feel or look like prosthetics. In addition, with modern techniques and high-quality materials on offer at our clinic, we can design implants that match the shape, size, and tone of your natural teeth so you won’t have to worry about their appearance or attracting the wrong kind of attention while socializing.
Where can I get biocompatible dental implants in Vista, CA?

As the leading oral health clinic in your area, from Rancho Guajome Adobe on the north to the south side and beyond the town limits, we’re here to help you anyway we can. If you have questions or concerns that need answering, we’re glad to offer help and guidance. Want to learn what to expect from our free implants consultation, what is osseointegration and why it matters, or which medical conditions disqualify you from All-on-4? Just go ahead and call or book your free initial assessment today!

 Ok, now that we’ve addressed the consultation fee, or lack thereof in our case, it’s time to move on to the All-on-4 consultation timeline and the next steps. Most evaluations take around 30 minutes, but they can extend to a full hour, depending on the case and the patient’s medical history. Consultations for dental implants typically include 3D imaging, diagnostics, and a discussion with the patient. X-rays or a cone beam scan can add to the overall consultation timeline. Keep in mind that your assessment may take longer if you have gum concerns or a complex medical history.
Ok, now that we’ve addressed the consultation fee, or lack thereof in our case, it’s time to move on to the All-on-4 consultation timeline and the next steps. Most evaluations take around 30 minutes, but they can extend to a full hour, depending on the case and the patient’s medical history. Consultations for dental implants typically include 3D imaging, diagnostics, and a discussion with the patient. X-rays or a cone beam scan can add to the overall consultation timeline. Keep in mind that your assessment may take longer if you have gum concerns or a complex medical history.














 Who do I turn to for quality dental implants in Mira Mesa and the surrounding area?
Who do I turn to for quality dental implants in Mira Mesa and the surrounding area?

 How do I find a reliable dental implant specialist in Mira Mesa and the surrounding area?
How do I find a reliable dental implant specialist in Mira Mesa and the surrounding area?

 Who do I turn to if I need high-quality All-on-4 implants in Scripps Ranch and the surrounding area?
Who do I turn to if I need high-quality All-on-4 implants in Scripps Ranch and the surrounding area?

 How do I find a reliable dental implant specialist in Scripps Ranch and the surrounding area?
How do I find a reliable dental implant specialist in Scripps Ranch and the surrounding area?